Symptoms of perimenopause – the lead up to menopause – can strike up to 15 years beforehand. For World Perimenopause Day, London GP Dr. Deyo Famuboni describes ten perimenopause symptoms to watch for
You’ve been going about your life, following your monthly routine, with no obvious changes in your body for the last five to ten years. Then suddenly, your period is late and your first thought is: ‘Am I pregnant?’.
You know this is highly unlikely as you have an effective contraceptive. You do a pregnancy test and it’s negative. Your period eventually shows up. So what’s going on?
Lifestyle intervention can help significantly with the perimenopause
You may be in perimenopause, the natural transition period women go through before the menopause. This is a natural step in a woman’s body towards permanent infertility.
The average age of menopause in the UK is around 52 but perimenopause can start at different ages and most women sometimes notice changes in their early forties, and occasionally in their mid 30s.
This is due to female hormone changes, mainly oestrogen, rising and falling unevenly.
Generally, the perimenopause should not be a cause for alarm. Lifestyle intervention can help significantly with perimenopausal symptoms.
This includes regular exercise and a diet rich in phytooestrogens. These are natural plant oestrogens found in foods such as soybeans, dark leafy green and cruciferous vegetables such as broccoli.
However, if it is interfering with your quality of life and wellbeing, then see your doctor. Depending on your symptoms, further tests may be carried out. Various medical therapies including hormone replacement and non hormonal options are available on prescription.
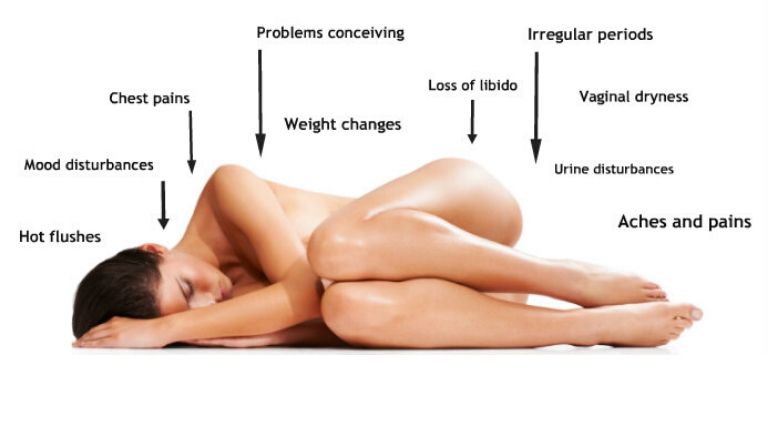
10 signs that you may be in perimenopause
#1 Irregular periods
The hormone changes affect your ovaries releasing an egg and this in turn can make your period longer or shorter or absent for a couple of months. These could be signs of early and late perimenopause respectively.
No periods for three months or more as well as very heavy periods, particularly if associated with feelings of tiredness or breathlessness warrant a review by your doctor, especially if you are under the age of 40.

#2 Hot flushes
Suddenly going hot and sweaty? This is common in the perimenopause and can vary in duration and intensity throughout the day and at night – this often contributes to insomnia and sleep disturbances.
This occurs as a result of the hormonal fluctuations and can be different for every woman. It can last anything between two years to 15 years.
Wearing breathable clothing such as cotton and staying hydrated can help in alleviating symptoms.
Avoiding other causes of hot flushes including being overweight, alcohol, excess caffeine, spicy foods, monosodium glutamate (a seasoning common in processed foods) and some medications can also help in alleviating symptoms.
#3 Mood disturbances
This can happen frequently with mood swings, as well as feeling irritable, short tempered or anxious. A change from your usual temperament can be a sign of the perimenopause as your hormones spike and sag.A lack of good quality sleep can also contribute to this.
Regular exercise and a healthy diet to ensure your blood sugar levels remain stable can help.
#4 Vaginal dryness
The hormone changes mean the vaginal wall decreases the amount of fluid it produces and also its elasticity. Some women can find it generally uncomfortable, others only notice it only during intercourse.
Also, the length of time it takes to get aroused increases with age. Using vaginal lubricants can alleviate this.
#5 Urine disturbances
In general, women are prone to urine infection because of our anatomy. This can happen for the first time during the perimenopause or increase in frequency. You might notice urine frequency and pain.
This warrants a review from a healthcare professional. A decreased ability to hold urine can also happen. This is because the elasticity and tone decreases.
Ways of preventing this includes passing urine afterintercourse, using lubricants and doing regular pelvic floor exercises.
#6 Loss of libido
There are various causes for this and the mood changes, lack of sleep and decreased arousal time can certainly contribute. However many women have no problems with this.
#7 Problems conceiving
Ovulation decreases and this leads to fertility problems. It can take up to one year to fall pregnant naturally, however if you are in your very late 30s or early forties and have trouble conceiving, it is worth seeking medical advice sooner.
Using contraception until 12 months after your last period is advisable if you do do not want to fall pregnant.
#8 General aches and pains
As oestrogen decreases, the body cannot replace bone as efficiently. The ligaments and cartilages are also affected. Research also suggests that the hormone changes are associated with the development of osteoarthritis.
Aches and pains can also be a sign that your bones are getting thin due to osteoporosis. Getting adequate calcium and vitamin D and exercising to strengthen the bones and muscles can help to prevent this.
Several studies have looked at the use of glucosamine for pains and though individual women have reported improvement in their symptoms, evidence for its use is limited.
#9 Weight changes
There are several contributory factors for this. This includes the metabolism and our ability to build muscle slowing down as well as higher levels of stress due to lack of sleep and worry about other signs mentioned above.
Stress can increase weight as elevated levels of the stress hormone cortisol can lead to weight gain around the middle. Improving the underlying cause is therefore needed.
Regular exercise and a healthy diet, with particular attention to your nutrient to calorie ratio can help negate weight gain. This is because you use up less calories as you get older.
A sudden increase in weight warrants a visit to your doctor.
#10 Chest pain
As oestrogen levels drops, the cholesterol and sugar level in the body increases. The heart and vessels also become more stiff. This puts you at risk of heart disease as it contributes to clogging up the blood vessels.
Left sided chest discomfort, especially on exertion requires urgent medical attention.

After graduating from the University of Edinburgh, she went on to do further training within a wide range of medical specialities including obstetrics and gynaecology.
She has spent time working abroad as well as within the NHS and private sectors in the UK.
She is a member and clinical advisor of the Royal College of General Practitioners and a diplomate of the Royal College of Obstetrics and Gynaecology, Royal College of Paediatricians and the Faculty of Sexual and Reproductive Health.
She also has a strong interest in nutrition and health and blogs at doctordeyo.com
Follow Dr Deyo on Instagram.
Relevant Healthista content:
How to destress – the breathing technique this Instagram yoga star wants you to know
Menopause symptoms? Here’s how these celebs dealt with theirs
Other Healthista content you might like:
PMS symptoms? These 4 natural remedies will help
3 healthy recipes this Instagram super-medic swears by
7 surprising hacks for a good night’s sleep
WIN £250 spa break plus beauty products worth over £70
Tired All the Time? 7 signs you need an energy makeover
Like this article? Sign up to our newsletter to get more articles like this delivered straight to your inbox.